General Dentistry
Crowns
 Over time our teeth begin to weaken and become more susceptible to problems such as decay, cracks, discoloration and others. If you feel your smile isn’t what it once was, crowns can help you recover your smile. If your dentist notices that a tooth is decayed or seems weakened/cracked a crown may be necessary to make sure that there are no additional problems with the tooth. In cases like this a filling or bonding will not be sufficient.
Over time our teeth begin to weaken and become more susceptible to problems such as decay, cracks, discoloration and others. If you feel your smile isn’t what it once was, crowns can help you recover your smile. If your dentist notices that a tooth is decayed or seems weakened/cracked a crown may be necessary to make sure that there are no additional problems with the tooth. In cases like this a filling or bonding will not be sufficient.
Crowns can be made from porcelain, porcelain fused to metal, or a full gold crown. To maintain a natural look and feel a porcelain finished crown is best, as it can be matched to the shade of your other teeth. This will allow it to blend in and appear just like one of your natural teeth.
The process of installing a crown takes 2-3 visits to the dentist. On the first visit the tooth will be reshaped by filing down the enamel so that the crown can be placed over it. You will be given a local anesthetic before this part of the procedure so that you do not experience any discomfort. Once the tooth has been reshaped, a mold will be taken of that tooth and the surrounding teeth. This mold will be sent to a dental lab so that your new crown can be made so that it fits in the spot created for it and looks the same relative to the surrounding teeth. Before leaving, your dentist will fit you with a temporary crown until your permanent crown is ready.
The crown takes about 2-3 weeks to be returned to your dentist. At this time you will have another appointment to place and fit the permanent crown. You will again have a local anesthetic to numb the area and the tooth will be placed using a cement to ensure the tooth sets in place. When you look in the mirror, you will see your old smile back. Crowns are durable and will usually last about 10-15 years. You should care for it as you would any of your other teeth with regular brushing and flossing. Call us today if you would like to learn more about how crowns can help restore your smile.
Dentistry for Diabetes
 Diabetes can cause serious problems in your mouth. You can do something about it.
Diabetes can cause serious problems in your mouth. You can do something about it.
If you have diabetes, make sure you take care of your mouth. People with diabetes are at risk for mouth infections, especially periodontal (gum) disease. Periodontal disease can damage the gum and bone that hold your teeth in place and may lead to painful chewing problems. Some people with serious gum disease lose their teeth. Periodontal disease may also make it hard to control your blood glucose (blood sugar).
Other problems diabetes can cause are dry mouth and a fungal infection called thrush. Dry mouth happens when you do not have enough saliva—the fluid that keeps your mouth wet. Diabetes may also cause the glucose level in your saliva to increase. Together, these problems may lead to thrush, which causes painful white patches in your mouth.
If your diabetes is not under control, you are more likely to develop problems in your mouth. The good news is you can keep your teeth and gums healthy. By controlling your blood glucose, brushing and flossing every day, and visiting a dentist regularly, you can help prevent serious problems in your mouth.
Take steps to keep your mouth healthy. Call your dentist when you notice a problem.
If you have diabetes, follow these steps:
- Control your blood glucose.
- Brush and floss every day.
- Visit your dentist regularly. Be sure to tell your dentist that you have diabetes.
- Tell your dentist if your dentures (false teeth) do not fit right, or if your gums are sore.
- Quit smoking. Smoking makes gum disease worse. Your physician or dentist can help you quit.
Take time to check your mouth regularly for any problems. Sometimes people notice that their gums bleed when they brush and floss. Others notice dryness, soreness, white patches, or a bad taste in the mouth. All of these are reasons to visit your dentist.
Remember, good blood glucose control can help prevent mouth problems.
Extractions
 Wisdom teeth extractions are a fairly common procedure. Wisdom teeth often cause problems as they are trying to protrude through the gums. When a wisdom tooth is impacted, it means the tooth is coming in at an angle and not straight through the gum line. This can cause pain, the tooth can come in unevenly, or the tooth may only emerge partially.
Wisdom teeth extractions are a fairly common procedure. Wisdom teeth often cause problems as they are trying to protrude through the gums. When a wisdom tooth is impacted, it means the tooth is coming in at an angle and not straight through the gum line. This can cause pain, the tooth can come in unevenly, or the tooth may only emerge partially.
When a wisdom tooth only emerges partially a flap of skin, called an operculum, may form over the tooth. This can make the tooth hard to clean, and pieces of food may be caught under the skin. This makes it easy for an infection, called pericoronitis, to develop. It will usually go away on its own, but it causes swelling and pain in the area.
Impacted teeth and wisdom teeth that can potentially cause problems, like infections, need to be removed. Extractions can range from a single tooth, to removing all four wisdom teeth at once. Based on the preference of the doctor and/or the patient, a local anesthetic could be used to numb the areas where the teeth will be extracted. Others will prefer to go under a general anesthetic so that they will be sedated during the procedure.
The gum tissue around the wisdom tooth is cut open to reveal the tooth. The tooth is loosened by gripping it tightly and wiggling it back and forth until it can be lifted out of the gums. Sometimes a tooth may be impacted so tightly that it cannot be simply lifted out of the gums. In cases like this the tooth will be broken up into pieces first before being removed. Depending on the incision and extraction site, sutures may be needed to close the area. Soluble sutures are the best option, which will dissolve on their own.
After the surgery you will need to rest. You need to be driven home by a friend or family member because of the anesthesia. You can expect for the extraction site to bleed for a little while after the surgery. Gauze will be applied at the completion of the surgery, and you will need to change it when it becomes soaked. If bleeding continues for longer than 24 hours you should call your dentist. Rest when you return home, but do not lie flat. This could prolong the bleeding. Prop your head up on a pillow when lying down. Your dentist will prescribe you pain medication, so if you become sore take as directed. You can also use an ice pack for the pain. Your dentist might also provide you with a cleaning solution to clean the extraction site.
You will be limited to soft foods for a few days after your surgery. Some recommended foods are:
- Gelatin
- Pudding
- Yogurt
- Mashed Potatoes
- Ice Cream
- Thin Soups
- ...and other food you can eat without chewing.
When drinking, make sure you do not use a straw. The sucking motion can loosen your sutures and slow the clotting process. The same goes for smoking. If you have prolonged pain, bleeding, irritation, or don't feel that the extraction site is healing properly call your dentist for a follow up.
Dental Hygiene and Periodontal Health
 While at our office, we make sure that you receive the highest level of service and ensure that our dental work is of the highest quality. To ensure that you maintain great oral health, this level of quality needs to extend into your personal oral hygiene routine. We can help you establish a dental hygiene routine that will keep your teeth healthy and white. If you have any questions about your current hygiene plan please ask us.
While at our office, we make sure that you receive the highest level of service and ensure that our dental work is of the highest quality. To ensure that you maintain great oral health, this level of quality needs to extend into your personal oral hygiene routine. We can help you establish a dental hygiene routine that will keep your teeth healthy and white. If you have any questions about your current hygiene plan please ask us.
Your teeth are not the only important part of your mouth. Your gums are essential to oral hygiene as well. We can provide periodontal cleanings and treatment, or refer you to one of our recommended specialists. Please let us know if you have any questions.
Extraction Site Preservation
 When removing a tooth it is important to consider what will be done with the empty space after that tooth is removed. Wisdom teeth are in the back of the mouth, so that site will heal on its own with no complications. If it is necessary to remove another tooth, plans must be made. If a tooth is removed and nothing is done with the extraction site, the jaw bone will degenerate and change shape during healing and can cause your teeth to shift. This can create problems in your bite and affect your ability to speak and chew.
When removing a tooth it is important to consider what will be done with the empty space after that tooth is removed. Wisdom teeth are in the back of the mouth, so that site will heal on its own with no complications. If it is necessary to remove another tooth, plans must be made. If a tooth is removed and nothing is done with the extraction site, the jaw bone will degenerate and change shape during healing and can cause your teeth to shift. This can create problems in your bite and affect your ability to speak and chew.
If you want to fill the space with a dental implant, a sturdy jaw bone is necessary to install the implant. If you opt for a dental bridge, the bridge must be molded and placed before the teeth shift.
Your dentist is always open to a conversation on what you would like to do with your extraction site before removing a tooth. They will be able to make a recommendation and layout a treatment plan. Make sure to schedule follow up appointments to properly care for your extraction site.
Inlays and Onlays
 Inlays and onlays are often referred to as partial crowns. They use the existing tooth as a base and fit the inlay or onlay onto the tooth. This is done to strengthen the tooth, restore its shape, and prevent further damage. An inlay is done when there is no damage to the cusps of the tooth and the inlay can be placed right on the tooth. An inlay is used when the damage is a little more extensive.
Inlays and onlays are often referred to as partial crowns. They use the existing tooth as a base and fit the inlay or onlay onto the tooth. This is done to strengthen the tooth, restore its shape, and prevent further damage. An inlay is done when there is no damage to the cusps of the tooth and the inlay can be placed right on the tooth. An inlay is used when the damage is a little more extensive.
The decayed area of the tooth is first removed during the procedure. A mold of the tooth is then taken and sent to a dental lab. They create a restoration made from porcelain, gold, or a composite resin. The restoration takes about 2-3 weeks to make, so a temporary inlay or onlay will be placed on the tooth for that time. During your next visit the inlay or onlay will be placed into your mouth and set with cement. Your tooth will look natural and you or anyone else won't be able to tell the difference.
TMJ
 TMJ is the acronym for temporomandibular joint, which connects your lower jaw (the mandible) to your skull at the temporal bone. This joint controls many jaw functions, like chewing. If the chewing muscles or the joint itself are causing you pain you may have temporamandibular disorder, or TMD. TMD can be caused by stress, continual clenching of the jaw muscles, or teeth grinding.
TMJ is the acronym for temporomandibular joint, which connects your lower jaw (the mandible) to your skull at the temporal bone. This joint controls many jaw functions, like chewing. If the chewing muscles or the joint itself are causing you pain you may have temporamandibular disorder, or TMD. TMD can be caused by stress, continual clenching of the jaw muscles, or teeth grinding.
Some of the symptoms of TMD are:
- Pain when opening or closing mouth
- Trouble chewing
- Jaw becoming stuck open or shut
- Headaches or ear pain
- Clicking or popping sounds when opening your mouth
- Teeth Grinding
Many of these symptoms can often be associated with other health problems, so only a medical professional can tell you if it is due to TMD. Teeth grinding is an especially problematic symptom because it can lead to further problems. Prolonged teeth grinding, or bruxism, can cause enamel to wear off teeth and expose dentin. This material is softer than enamel and more susceptible to decay. Sensitivity to hot and cold food or drink may also develop from excessive teeth grinding.
If you suspect you may have TMD come in for a consultation. We can help diagnose you and provide relief for your symptoms. Pain relievers and hot/cold compresses are short term methods to provide relief for pain symptoms. A night guard can be used to help prevent or lessen the effects of teeth grinding at night. This can lead to a more permanent solution. In very severe cases of TMD surgery may be required, but behavioral treatments to change the way you use your jaw muscles are usually enough to provide relief.
Night Guards
 Many people are afflicted with bruxism, or teeth grinding. Some people may do this consciously during the day, but it is a larger problem at night while you are asleep. Grinding your teeth can damage enamel, wear down teeth, cause jaw pain, or irritate your gums. The noise from teeth grinding can also disturb your spouse's sleep if loud enough.
Many people are afflicted with bruxism, or teeth grinding. Some people may do this consciously during the day, but it is a larger problem at night while you are asleep. Grinding your teeth can damage enamel, wear down teeth, cause jaw pain, or irritate your gums. The noise from teeth grinding can also disturb your spouse's sleep if loud enough.
If you grind your teeth you should consider a night guard. The night guard, which is very similar to a mouth guard worn by athletes, provides a barrier between your top and bottom teeth while you sleep. All night guards are custom fitted for comfort and to allow for proper breathing. Your dentist will take an impression of your teeth and have the night guard created by a dental lab. Night guards are very durable and can be used for up to 10 years.
There are also some things that you can do to try to stop teeth grinding. You can train your jaw to be free and easy rather than clenched. Refrain from chewing gum or on other objects like pens. You should also avoid alcoholic drinks and drinks with caffeine, as these can increase the likelihood you will grind your teeth. If you suspect you might be grinding your teeth at night set up an appointment with us today.
White Fillings (Bonding)
 After the anesthesia wears off your teeth will likely be sensitive. You should avoid hot and cold food or drink for the next few days. After that initial period, your treated teeth will feel as good as new. Continue your normal hygiene plan to ensure that your fillings last for a long time.
After the anesthesia wears off your teeth will likely be sensitive. You should avoid hot and cold food or drink for the next few days. After that initial period, your treated teeth will feel as good as new. Continue your normal hygiene plan to ensure that your fillings last for a long time.
Extractions
 After the surgery you will need to rest. You need to be driven home by a friend or family member because of the anesthesia. You can expect for the extraction site to bleed for a little while after the surgery. Gauze will be applied at the completion of the surgery, and you will need to change it when it becomes soaked. If bleeding continues for longer than 24 hours you should call your dentist. Rest when you return home, but do not lie flat. This could prolong the bleeding. Prop your head up on a pillow when lying down. Your dentist will prescribe you pain medication, so if you become sore take as directed. You can also use an ice pack for the pain. Your dentist might also provide you with a cleaning solution to clean the extraction site.
After the surgery you will need to rest. You need to be driven home by a friend or family member because of the anesthesia. You can expect for the extraction site to bleed for a little while after the surgery. Gauze will be applied at the completion of the surgery, and you will need to change it when it becomes soaked. If bleeding continues for longer than 24 hours you should call your dentist. Rest when you return home, but do not lie flat. This could prolong the bleeding. Prop your head up on a pillow when lying down. Your dentist will prescribe you pain medication, so if you become sore take as directed. You can also use an ice pack for the pain. Your dentist might also provide you with a cleaning solution to clean the extraction site.
You will be limited to soft foods for a few days after your surgery. Some recommended foods are:
- Gelatin
- Pudding
- Yogurt
- Mashed Potatoes
- Ice Cream
- Thin Soups
- ...and other food you can eat without chewing.
When drinking, make sure you do not use a straw. The sucking motion can loosen your sutures and slow the clotting process. The same goes for smoking. If you have prolonged pain, bleeding, irritation, or don't feel that the extraction site is healing properly call your dentist for a follow up.
Post-Op Instructions
 It is important to follow instructions after you have oral surgery to ensure proper healing and to avoid complications. As a rule of thumb, you should always wait two hours after surgery before eating to let the anesthesia wear off. Trying to eat before this could result in soft tissue damage because you are not able to feel all of your mouth. The instructions found below are guidelines. After your surgery the doctor or dental assistant will give you full instructions on how to properly recover from surgery.
It is important to follow instructions after you have oral surgery to ensure proper healing and to avoid complications. As a rule of thumb, you should always wait two hours after surgery before eating to let the anesthesia wear off. Trying to eat before this could result in soft tissue damage because you are not able to feel all of your mouth. The instructions found below are guidelines. After your surgery the doctor or dental assistant will give you full instructions on how to properly recover from surgery.
Arestin: Fighting infection where it starts
 You may have heard about gum disease, also known as "periodontitis" or "periodontal disease." Maybe a dental professional or hygienist recently told you that you have this infection.
You may have heard about gum disease, also known as "periodontitis" or "periodontal disease." Maybe a dental professional or hygienist recently told you that you have this infection.
But do you really know the difference between periodontal disease and other types of complications that can affect your mouth, such as gingivitis?
Do you know why it's so important to treat periodontal disease-and why brushing and flossing alone won't do the trick?
Most importantly, did you know that periodontal disease is today's #1 cause of tooth loss among American adults? Or that, although a causal relationship between periodontal disease and an elevated risk for systemic events has not been established, recent data suggest a possible association between periodontal disease and other health issues including cardiovascular disease, diabetes, and preterm low birth-weight babies?
Fight infection right where it starts
ARESTIN® (minocycline hydrochloride) Microspheres, 1 mg is an effective antibiotic treatment that comes in powder form. This powder is placed inside infected periodontal pockets just after the dental professional finishes the scaling and root planing (SRP) procedure.
Periodontal (gum) Disease
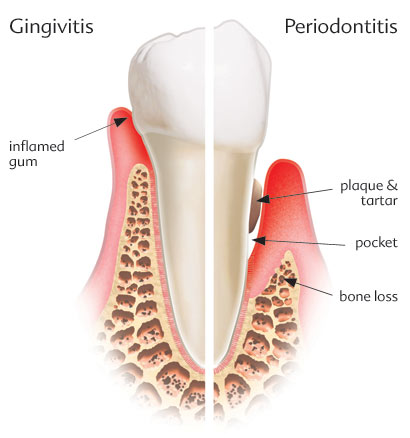 Periodontal (gum) disease is insidious. It is an infection of the gums that starts out as plaque, an opaque film on the teeth that hardens to form tartar. As tartar accumulates, it harbors bacteria that attack the soft tissue around the gums. This is the early stage of gum disease known as Gingivitis. Left untreated, Gingivitis becomes Periodontitis which ultimately destroys the tissue surrounding your teeth AND the bone that holds your teeth in place. Except for bad breath and gums that bleed, there are very few early warning signals. The disease advances silently, often without pain, and before you know it, you are losing your teeth and you don't know why.
Periodontal (gum) disease is insidious. It is an infection of the gums that starts out as plaque, an opaque film on the teeth that hardens to form tartar. As tartar accumulates, it harbors bacteria that attack the soft tissue around the gums. This is the early stage of gum disease known as Gingivitis. Left untreated, Gingivitis becomes Periodontitis which ultimately destroys the tissue surrounding your teeth AND the bone that holds your teeth in place. Except for bad breath and gums that bleed, there are very few early warning signals. The disease advances silently, often without pain, and before you know it, you are losing your teeth and you don't know why.
Tooth loss is only the most obvious indicator of gum disease. Scientific research has discovered linkage between gum disease and stroke, heart disease, diabetes - even an increased risk for pregnant women. When your gums become diseased, your entire immune system is weakened.
In the past, fear of painful dental surgery has kept people with gum disease from seeking the care they needed. Well, those days are gone forever.
Scaling & Root Planing
 Gingivitis is a generative disease that left untreated, will cause significant tooth and gum deterioration. Just the word gingivitis can strike panic in a patient’s mind. The reality is that the treatment is simple and performed right in your dentist’s office.
Gingivitis is a generative disease that left untreated, will cause significant tooth and gum deterioration. Just the word gingivitis can strike panic in a patient’s mind. The reality is that the treatment is simple and performed right in your dentist’s office.
Plaque and tarter that sits on the teeth provides an environment, which allows bacteria to thrive and multiply. The bacteria cause the gums to become inflamed and bleed. The condition becomes more noticeable when you brush your teeth or sometimes when you eat. These are signs of the early stage of gingivitis. Gingivitis is easily treated by having the hygienist scaling and polishing the teeth. If gingivitis is left untreated, the condition will progress and the roots will need a planing. The difference between scaling and root planing is simple. Scaling is the removal of the dental tartar from the tooth surface Root planing is the process of smoothening the root surfaces and removing the infected tooth structure.
As a non-surgical procedure, scaling and planing is performed without any anesthesia, in the dentist’s office. While the procedure is usually painless, advanced stages of gingivitis may make it necessary to numb the area for complete comfort. Deep scaling and root planing is usually broken down into one section of the mouth per appointment. This allows for adequate healing time, and reduces the time for each appointment.
After this procedure your gums will probably be slightly sore and irritated for a few days. You should rinse your mouth with warm salt water (1 tsp salt/8 oz water) 2-3 times a day. This will relieve the pain and cleanse the area. Brushing and flossing should be continued right after the procedure, but you should brush gently so that you do not further irritate the area. If you experience any swelling or stiffness in the area you can place a cold compress on the area and take some pain relieving medicine. Avoid any hard or chewy foods for 2-3 days after the surgery to ensure the area heals correctly. If you continue to experience pain or swelling after a few days contact your dentist.
Sealants
 Sealants are a great way to protect against tooth decay and cavities on your back teeth (molars). These are the teeth that are most vulnerable to cavities and decay because they are used in the chewing process, and are the most difficult to reach and clean. Molars first come in at around 5-7 years of age, with a second set coming in between the ages of 11-14. It is best to have a sealant placed when the molars first come in to ensure they are protected early.
Sealants are a great way to protect against tooth decay and cavities on your back teeth (molars). These are the teeth that are most vulnerable to cavities and decay because they are used in the chewing process, and are the most difficult to reach and clean. Molars first come in at around 5-7 years of age, with a second set coming in between the ages of 11-14. It is best to have a sealant placed when the molars first come in to ensure they are protected early.
To place a sealant an adhesive is first applied to the teeth. The sealant is then placed over the adhesive as a liquid, as if it is painted right onto the tooth. The liquid then hardens and creates a barrier between your tooth and any plaque, food particles, and bacteria. Sealants last for about 10 years and can be reapplied if necessary.
Root Canal (Endodontics)
 Endodontics is the dental specialty that deals with the nerves of the teeth. Root canals are probably the most notorious procedure in dentistry and the most common procedure relating to endodontics. When a tooth becomes infected it is usually related to the nerves in the root of the tooth. The infected nerves need to be removed. If left untreated an infection can turn into an abscess, which is a much more serious problem that includes bone loss in the jaw.
Endodontics is the dental specialty that deals with the nerves of the teeth. Root canals are probably the most notorious procedure in dentistry and the most common procedure relating to endodontics. When a tooth becomes infected it is usually related to the nerves in the root of the tooth. The infected nerves need to be removed. If left untreated an infection can turn into an abscess, which is a much more serious problem that includes bone loss in the jaw.
The area around the tooth is numbed with a local anesthetic to start the procedure. The dentist will then drill down into the tooth to create an opening into the canal. They will then be able to remove infected tissue and clean the canal. After the infection has been removed, the space if filled with a sealant called gutta percha. It is highly recommended that a tooth that has undergone a root canal is fitted with a crown. This will improve the appearance of the tooth, and will also make it much more likely that the root canal is successful.
"Root canal" has become a scary term for dental patients to hear, but the benefits of the procedure and advances in dental technology have made it much less "scary". Local anesthetics and proper pain medication allow the procedure to be performed with little to no pain in most cases. There may be some soreness following the procedure, but that is normal for most dental procedures. Over the counter painkillers are usually enough to relieve any pain afterwards, but your dentist may prescribe medication. The procedure will also relieve you from pain caused by the infection allowing you to enjoy all the foods you love without any pain from heat, cold, or biting too hard.
You can expect soreness after a root canal procedure for a few days. You should avoid chewing on the side of your mouth where the procedure was performed so you do not irritate the area and also to ensure that the temporary restorative material properly sets. You will also need to take an antibiotic to treat any remaining infection in your tooth. If you notice an increasing amount of pain or tenderness, a reaction to the medication, or the loss of the temporary restoration (filling) call your dentist immediately.
Nitrous Oxide
 Nitrous oxide has been the primary means of sedation in dentistry for many years. Nitrous oxide is safe, the patient receives 50 – 70 percent oxygen with no less than 30 percent nitrous oxide. It is a sweet smelling, non-irritating, colorless gas which is inhaled. The patient is able to breathe on his or her own and remain in control of all bodily functions.
Nitrous oxide has been the primary means of sedation in dentistry for many years. Nitrous oxide is safe, the patient receives 50 – 70 percent oxygen with no less than 30 percent nitrous oxide. It is a sweet smelling, non-irritating, colorless gas which is inhaled. The patient is able to breathe on his or her own and remain in control of all bodily functions.
The patient may experience mild amnesia and may fall asleep not remembering all of what happened during their appointment.
There are many advantages to using nitrous oxide.
The depth of sedation can be altered at any time to increase or decrease sedation.
There is not after-effect such as a “hangover”.
Inhalation sedation is safe with no side effects on your heart or lungs.
Inhalation sedation is very effective in minimizing gagging.
It works rapidly reaching the brain within 20 seconds. In as few as two to three minutes, it’s relaxation and pain-killing properties develop.
Reasons Not To Use Nitrous Oxide
Though there are no major contraindications to using nitrous oxide, you may not want to use it if you have emphysema, chest problems, multiple sclerosis, a cold, or other difficulties with breathing.
You may want to ask your dentist for a five-minute trial to see how you feel with this type of sedation method before proceeding.
VIP Ammenities
 Our office offers amenities and interesting extras to make each visit with us an enjoyable experience. Our goal is to provide high quality dental care while putting you in the most comfortable setting possible. Our facility is one whose dental program is run under the strict supervision of a licensed dentist.
Our office offers amenities and interesting extras to make each visit with us an enjoyable experience. Our goal is to provide high quality dental care while putting you in the most comfortable setting possible. Our facility is one whose dental program is run under the strict supervision of a licensed dentist.
Today's Patient can enjoy the following VIP luxuries:
- Head Rest Pillows
- Blankets
- Flat Screen TV's
- Soothing Music
- Laughing Gas (Nitrous Oxide)

